Q&A: Dr. Mona Orady

Minimally invasive gynecologic surgery is transforming the treatment of common gynecologic conditions.
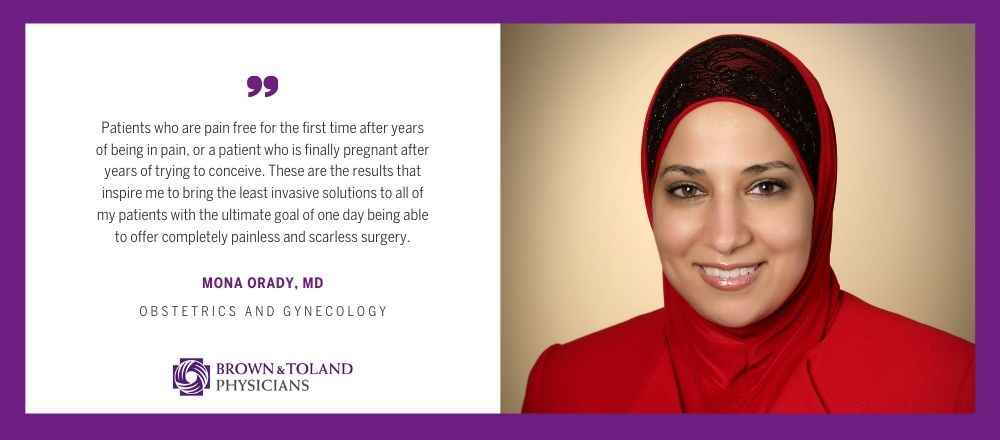
Compared with traditional, or “open” surgery, minimally invasive laparoscopy and robotic-assisted surgery involves one or a few tiny incisions that surgeons use to insert surgical equipment and a camera for viewing. The procedure is then precisely performed with these tiny instruments on the inside, thus avoiding the need for a large incision even to perform complex procedures such as hysterectomy, myomectomy, or endometriosis excision. Brown & Toland gynecologic surgeon, Mona Orady, MD, sat down with us recently to discuss these techniques and what inspires her to continue pushing the limits of what’s possible in minimally invasive gynecologic surgery.
What is minimally invasive gynecologic surgery? What is the goal?
In short, minimally invasive (or laparoscopic) gynecologic surgery uses techniques and technology designed to help a patient in a way that has minimal impact on her – meaning minimal scarring, minimal pain, minimal recovery time. The goal is to have women return to their normal lives as quickly as possible. Minimally invasive gynecologic surgery can be used to correct a problem, resolve pain or treat fertility issues.
What is robotic-assisted surgery? When is it used?
Robotic gynecologic surgery is an advanced form of minimally invasive surgery where computer-assisted robotic instruments, precisely controlled by the surgeon, are used to assist in certain procedures. The surgical robot helps perform even the most complex and delicate procedures through very small incisions with incredible precision. It also allows surgeons to operate in very tight spaces in the body that would otherwise only be accessible through “open” surgery. In fact, the enhanced 10X magnified high-definition vision and the tiny robotic “hands” allow these procedures to be performed even more precisely and more delicately than open or traditional laparoscopic surgery. Robotic surgery can be used for many procedures, including hysterectomy, removal of fibroids with uterine reconstruction, removal of ovarian cysts, as well as to remove and treat endometriosis.
So, patients can usually opt for a minimally invasive procedure instead of “open” surgery?
Yes. Today, open surgeries for hysterectomy and other gynecologic issues are almost always unnecessary. Open surgeries are now mostly reserved for patients who have medical complications not allowing laparoscopy, or patients with advanced cancers when multiple procedures are performed during a single surgery to remove the cancer. Most benign gynecologic surgeries, even the most complex, can now be performed with robotic surgery with expert surgeons who are pushing the limits of minimally invasive surgery.
I’d also like to add that there are also many alternatives to hysterectomy to resolve a problem without removing the uterus. Open hysterectomy used to be the standard for the treatment of many gynecologic issues. Now, minimally invasive fibroid removal and endometriosis resection, for example, can be done so that the removal of the uterus is unnecessary, preserving or even enhancing a woman’s fertility.
We’re talking in March, which happens to be Endometriosis Awareness Month. What can you tell us about the condition and the options to treat it?
Endometriosis is an inflammatory condition where endometrial tissue (tissue similar to the lining of the uterus) grows outside of the uterus. Endometriosis can cause pain — sometimes severe — especially during menstrual periods. As the disease progresses, patients can also experience gastrointestinal issues, bloating, pain with bowel movements or urinary symptoms such as frequency, urgency, or the need to wake up at night to go to the bathroom. Pain with sex is also often a symptom of endometriosis. Fertility problems also may develop over time.
It is estimated that 1 in 10 women in the United States has endometriosis. Unfortunately, because of a lack of awareness, and the complex symptom profile for endometriosis that can present differently in different individuals, it often takes six to 10 years and three to five physicians for an endometriosis patient to get diagnosed. Most women also do not know that very painful periods are not normal and are often a sign of an underlying problem. For this reason, endometriosis awareness is so important.
The good news is that after an accurate diagnosis, endometriosis can be precisely removed using minimally invasive surgery techniques including mini/micro laparoscopy, laparoscopy with Co2 laser, or robotic surgery to help resolve the patients’ pain or fertility issues and restore her normal life and relationships. If endometriosis is also involving multiple organs, I often will use a team of surgeons to completely remove the disease.
For patients who do not desire surgery at the present time, there are some medications that help suppress the active symptoms of the condition until surgery is needed. For patients with pelvic pain, painful periods, pain with sex, or recurrent monthly gastrointestinal or urinary symptoms, I encourage them to seek evaluation with an expert in endometriosis since endometriosis is often not well understood by physicians who do not care for these patients on a daily basis.
How did you become interested in gynecologic surgery as a specialty?
I knew that I wanted to be a doctor when I was 4 years old and I knew I wanted to be a gynecologist by the time I was 9, so it’s been my passion for a very long time. My first year of medical school was when I became interested in gynecological surgery, thanks to my mentor – watching him perform surgery was just amazing. Being able to resolve a woman’s pain, bleeding or fertility issues with a single surgery for me seemed almost miraculous. As I progressed in my career, my passion for helping women only increased.
I travelled around the world working, teaching, and learning from gynecologic minimally invasive surgeons with expertise in fibroids and endometriosis. I started pushing the limits of laparoscopic and robotic surgery and found that most conditions could be treated with minimally invasive surgery. I found almost no reason to perform an open surgery. Over the last 20 years I have developed expertise in treating complex cases of fibroids and endometriosis, including fertility-sparing, and fertility-enhancing surgery, so that I can give women other options for treatment other than birth control pills and hysterectomy, which are usually the only two options given to patients with complex menstrual disorders. Being able to provide women with the opportunity to significantly improve their lives with a minimally invasive surgery with only one to two weeks of recovery time has been truly life-changing for both my patients and me. My only wish is that all women knew they had options other than sub-optimal treatment or having to continue to suffer in silence.
On a different note, I’ve heard that you’re an avid ice skater. How did that come about?
I was born in Ontario and earned my undergraduate and medical degrees there. When I started my residency at Ohio State, we would always have our annual Christmas party at the local ice rink. The first year, my chairman, who is also Canadian (and was skating circles around me) said to me “How can you be Canadian and not know how to ice skate?” So, I committed myself to learning how to skate before the following year’s party – and I did. Ever since then, it’s just been a great hobby. I love the freedom that the ice gives you.
What is it that continues to drive you in your career?
Every day I become aware of a success story or hear from a patient that I feel like I’ve truly made a difference in their life. Patients who are pain free for the first time after years of being in pain, or a patient who is finally pregnant after years of trying to conceive. These are the results that inspire me to bring the least invasive solutions to all of my patients with the ultimate goal of one day being able to offer completely painless and scarless surgery.
Brown & Toland physician, Mona Orady, MD, is an award-winning gynecological surgeon who is board certified in Obstetrics and Gynecology. With subspecialty expertise in minimally invasive surgery, including laparoscopic and robotic techniques, endometriosis, fibroids and reconstructive surgery, Dr. Orady offers individualized, comprehensive, and compassionate care to women of all ages. She travels the world teaching advanced surgery is the current president of the Society of Laparoscopic and Robotic Surgeons. She is currently director of Robotic Surgery Services at St. Francis Memorial Hospital in San Francisco and practices at Dignity Health Medical Group – San Francisco.
MEDICAL DISCLAIMER: The content of this Website or Blog is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this Website or Blog.
If you think you may have a medical emergency, call 911 immediately, call your doctor, or go to the emergency room/urgent care.
