Three Things a Palliative and Hospice Care Specialist Wants You to Know

Palliative care programs are designed to help people manage their symptoms from a serious illness. Although palliative care is part of hospice care, palliative care can also be offered much earlier and at the same time as curative care. Hospice care is comfort care without curative care and is available to patients during their last six months of life.
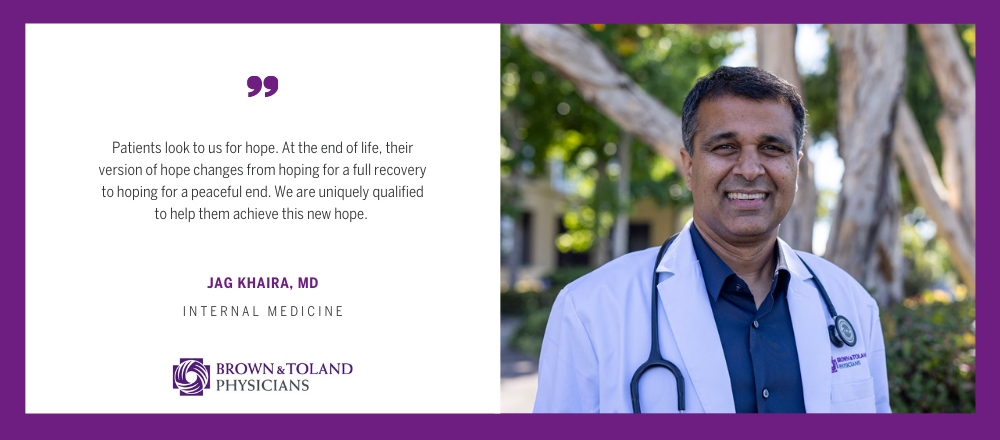
This Palliative Care Awareness Month, hospice and palliative care specialist Jag Khaira, MD, answers some common questions about this specialty.
What is the role of the family physician in palliative and hospice care?
Thanks to modern medicine, people are living longer with serious and complex illnesses. But today’s fragmented health care system makes it difficult to effectively treat people living with a serious illness.
Thus, the role of the family physician is key in providing continuity of care. Patients trust their family physician. Family physicians often provide patients with their first introduction to palliative care. They lead discussions regarding advance directive forms during annual wellness visits. And who better than the primary care physician? They often know the patient and family for the longest period.
As a hospice and palliative care specialist, I have been trained in supporting patients with quality-of-life, managing symptoms, emotional well-being and caregiver need. I also discuss person-centered advance care planning, which gives the patient a platform to have intimate conversations about their core values and beliefs. These conversations can lead to breakthroughs for some patients, which is very gratifying.
What are some of the misconceptions that people have about hospice and palliative care?
When I started my career as a primary care physician 20 years ago, I had misconceptions about the goals of hospice and palliative care. In fact, I did not know there was any difference between the two! In hospice care, patients understand that they are forgoing care such as ER visits, chemotherapy, etc. Palliative care is supportive care provided to patients with serious illness as they continue to receive aggressive care that is aimed toward a cure. In other words, palliative care is in addition to aggressive/usual care whereas hospice is instead of aggressive/usual care.
I used to feel that if my primary care patient went to hospice, they would feel as if I was “giving up” on them. Now I realize that their expectation is not for us to keep them alive forever, but to be there for them. Especially when they need us the most.
Are there clinical requirements to receive palliative care? Referral to hospice care?
While there are no strict clinical requirements to receiving palliative care, there are some common characteristics of the patients who would most benefit from it, such as a new cancer diagnosis, significant memory loss, heart and/or kidney failure, liver failure, a patient with COPD who is on oxygen, a patient who has had more than two hospitalizations in the past 12 months, limitations in activities of daily living, use of walkers or a hospital bed, multiple home health episodes, and nursing home stays. Many of these patients usually have less than five years of life.
To qualify for hospice care, patients need to have a terminal illness which a physician believe gives them less than six months to live. But sometimes patients will “graduate” from hospice care as the intensive treatment has improved their underlying issues such that they are no longer felt to be terminal.
The field of hospice and palliative medicine has its challenges, but I am grateful to be able to support my patients during their time of need. It goes without saying that there are moments of deep sorrow, but there are also moments of intimacy and love that provide fulfillment and hope.
Jagmohan S. Khaira, MD, is board certified in internal medicine and began his career as a medical student at Ross University School of Medicine in Portsmouth, Dominica. Upon graduation, he completed a residency at MetroHealth Medical Center, a leading teaching hospital of Case Western Reserve University School of Medicine in Cleveland. Dr. Khaira completed his postdoctoral clinical training at Loma Linda University Medical Center in Southern California.
Dr. Khaira is a founder of Marina Village Medicine in Alameda, Calif. He believes that building a strong relationship between a patient and their primary care doctor is at the core of getting and maintaining excellent medical care. For him, taking the time to get to know his patients is time well spent, and ultimately leads to the best outcomes.